Anterior cruciate ligament (ACL) injuries are among the most common and challenging knee injuries faced by athletes and active individuals alike. Navigating the path from diagnosis to recovery often brings uncertainty and a host of questions for patients. In our latest BMJ Blogs article, “The ACL Injury Journey – A Guide for Patients,” we delve into the essentials of understanding this injury, exploring treatment options, rehabilitation strategies, and what patients can expect at every stage. This comprehensive guide aims to empower those affected with clear, evidence-based information to help them take control of their recovery journey.
Understanding the Initial Diagnosis and Immediate Steps
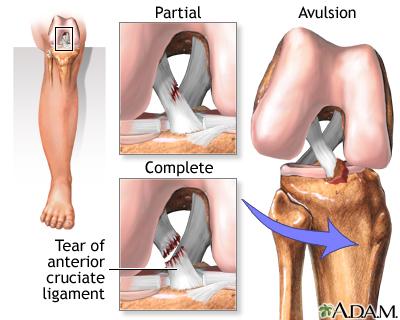
Following an ACL injury, the initial diagnosis is crucial for setting the course of treatment and managing patient expectations. Early assessment typically involves a combination of physical examinations and imaging tests, with MRI scans serving as the gold standard to confirm ligament damage. Healthcare professionals focus not only on the extent of the tear but also on any associated injuries to surrounding structures like the meniscus or cartilage, which can complicate recovery. At this stage, recognizing signs such as knee instability, swelling, and pain intensity aids clinicians in differentiating between partial and complete tears, shaping the urgency and type of intervention required.
Once the diagnosis is established, immediate management centers on minimizing further damage while preparing for rehabilitation. Patients are advised to engage in the RICE protocol-Rest, Ice, Compression, and Elevation-to control inflammation and pain. Immobilization through bracing may be recommended to stabilize the joint, especially in cases of complete rupture. To provide clarity, the table below summarizes key immediate steps:
| Step | Purpose | Patient Action |
|---|---|---|
| Rest | Prevent aggravation of injury | Avoid weight-bearing and strenuous activities |
| Ice | Reduce swelling and numb pain | Apply ice packs for 20 minutes every 2 hours |
| Compression | Limit fluid accumulation | Use elastic bandages or compression sleeves |
| Elevation | Facilitate fluid drainage | Keep knee elevated above heart level when possible |
Navigating Treatment Options and Making Informed Choices
Deciding on the most suitable path after an ACL injury involves weighing a variety of factors from personal lifestyle to long-term health outcomes. Surgery is often recommended for athletes and individuals seeking a return to high-impact activities, aiming to restore knee stability and prevent further damage. However, non-surgical approaches, including targeted physiotherapy and strength training, can be effective for patients with lower activity demands or those wishing to avoid operative risks. Each option carries its own timeline for recovery, potential complications, and impact on knee function, making personalized discussion with an orthopedic specialist essential.
Patients are encouraged to consider these key elements when exploring treatment options:
- Age and activity level: Younger, active patients may benefit more from reconstruction surgery; older or less active individuals might manage well conservatively.
- Knee stability and function: Persistent instability often calls for surgical intervention, whereas stable knees may adapt through rehabilitation.
- Recovery time and lifestyle needs: Surgery typically demands a longer recovery window, a critical factor for those balancing work or family commitments.
| Treatment Option | Pros | Cons | Typical Recovery |
|---|---|---|---|
| ACL Reconstruction Surgery | Restores knee stability; allows return to high-level sports | Involves surgical risks; longer rehab period | 6-12 months |
| Conservative Management | Avoids surgery; focuses on strengthening and mobility | Possible residual instability; limits high-impact activities | 3-6 months |
Rehabilitation Strategies for Optimal Recovery
Recovering from an ACL injury is a step-by-step process that demands patience, consistency, and professional guidance. Central to this journey is a well-structured rehabilitation program tailored to the individual’s injury severity and lifestyle. Early stages focus on reducing inflammation and regaining knee mobility through gentle range-of-motion exercises and isometric strengthening. As progress builds, the emphasis shifts towards restoring muscle strength, proprioception, and functional abilities, ensuring the knee can withstand daily activities and sporting demands.
Emerging evidence supports a multidisciplinary approach combining physical therapy, neuromuscular training, and gradual return to sport protocols. Patients benefit from incorporating:
- Progressive weight-bearing exercises to stimulate healing without overloading the joint
- Balance and agility drills to improve coordination and prevent re-injury
- Psycho-social support to address mental barriers common in recovery phases
| Rehab Phase | Key Focus | Typical Duration |
|---|---|---|
| Acute | Swelling control, pain management | 1-2 weeks |
| Strengthening | Muscle activation, range of motion | 3-8 weeks |
| Neuromuscular Training | Balance, proprioception | 8-16 weeks |
| Functional/Return to Sport | Sport-specific drills, confidence building | 16+ weeks |
Managing Expectations and Emotional Wellbeing Throughout the Process
Recovery from an ACL injury extends beyond physical healing; it deeply intertwines with your mental and emotional wellbeing. Setting realistic goals and understanding the typical timeline can prevent feelings of frustration and disappointment. Embrace patience, and remember that setbacks are often part of the journey, not a sign of failure. Incorporating regular mental health check-ins-whether through journaling, meditation, or professional support-can make a significant difference in maintaining a positive outlook.
It’s essential to maintain open communication with your healthcare team and loved ones, sharing your progress and concerns. Building a support network aids in managing the emotional rollercoaster that often accompanies rehabilitation. Consider these practical habits to nurture your emotional health:
- Celebrate small wins: Each milestone-be it increased mobility or pain reduction-is progress.
- Engage in social activities: Staying connected combats feelings of isolation.
- Develop alternative routines: Find enjoyable activities that don’t strain your knee but keep you active.
| Common Emotional Challenges | Recommended Coping Strategies |
|---|---|
| Frustration with slow progress | Set small, achievable goals; practice mindfulness |
| Fear of re-injury | Discuss concerns with physiotherapist; gradual exposure |
| Isolation during recovery | Join support groups; maintain social connections |
In Summary
As the understanding of ACL injuries continues to evolve, this guide offers patients a comprehensive roadmap through diagnosis, treatment options, and rehabilitation. Navigating the challenges of recovery can be daunting, but informed patients are better equipped to engage with healthcare providers and make decisions that suit their individual needs. With ongoing research and advancements in care, the journey from injury to recovery is becoming increasingly hopeful for those affected by ACL tears.