In a significant development for sports medicine and cardiology, new guidelines aimed at enhancing the interpretation of electrocardiograms (ECG/EKG) in athletes have been unveiled. These updated protocols promise to improve the accuracy of cardiac assessments, reducing false positives and ensuring timely identification of potentially life-threatening conditions. In this guest blog for BMJ Blogs, Dr Babette Pluim, a leading expert in sports cardiology, delves into the key changes and their implications for clinicians, athletes, and healthcare providers alike.
New Protocols Aim to Enhance Accuracy in Athlete ECG Interpretation
Recent advancements emphasize a more tailored approach when interpreting ECGs in athletes, recognizing the unique physiologic adaptations of the athletic heart. The new protocols integrate demographic factors such as age, ethnicity, and sport type, reducing false-positive diagnoses and ensuring that genuine cardiac abnormalities aren’t overlooked. By differentiating normal athletic remodeling from pathological changes, these guidelines aim to decrease unnecessary interventions and optimize athlete safety.
Key components of the updated interpretation framework include:
- Age and ethnicity-specific ECG criteria to better reflect population variances
- Sport-specific cardiac remodeling patterns incorporated into diagnostic thresholds
- Emphasis on a multidisciplinary review involving cardiologists and sports medicine experts
- Advanced algorithmic tools integrating clinical history and imaging for comprehensive assessment
| Protocol Aspect | Previous Standard | New Guideline |
|---|---|---|
| Interpretation focus | Generic athlete criteria | Individualized demographic data |
| False positive rate | Up to 20% | Reduced to under 10% |
| Multidisciplinary involvement | Occasional | Mandatory |
| Use of AI tools | Limited | Integrated analysis |
Addressing Common Diagnostic Challenges in Sports Cardiology
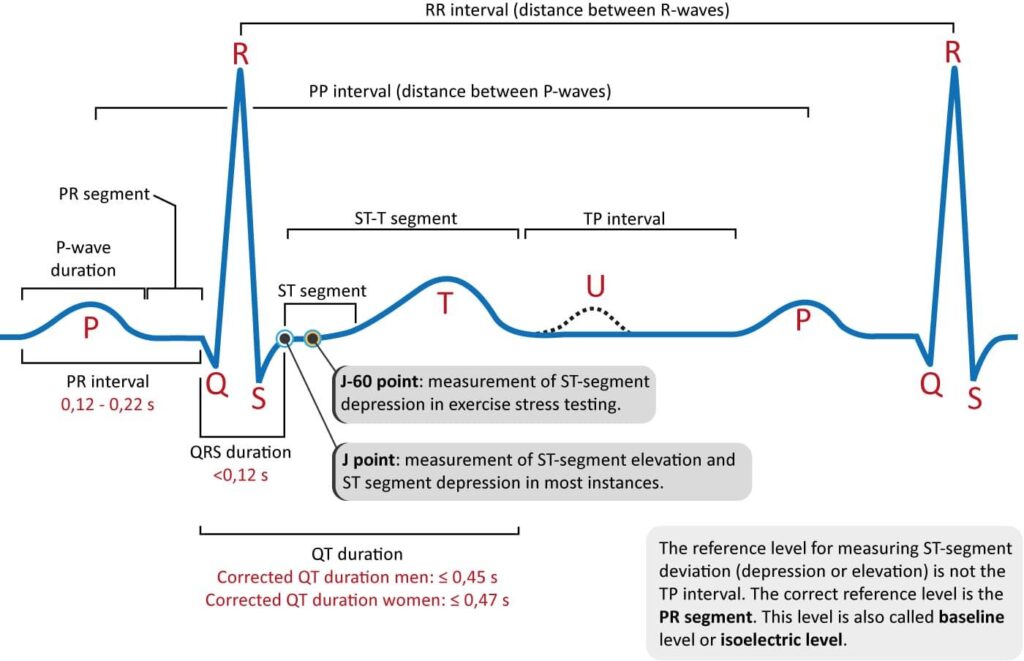
Accurate interpretation of ECGs in athletes presents unique challenges due to physiological adaptations from intense training that can mimic pathological findings. Distinguishing normal variants such as early repolarization or sinus bradycardia from potentially life-threatening conditions like hypertrophic cardiomyopathy requires a nuanced understanding beyond standard criteria. New recommendations emphasize a combination of athlete-specific ECG criteria and clinical context to reduce false positives and unnecessary investigations, streamlining the diagnostic pathway.
The updated guidelines advocate for an integrated approach using advanced imaging techniques and structured risk stratification tools alongside ECG findings. Key points include:
- Recognition of ethnic and sport-specific ECG patterns
- Utilization of echocardiography and cardiac MRI when indicated
- Standardized interpretation frameworks to improve inter-reader reliability
- Prioritizing shared decision-making with athletes to contextualize findings
| Challenge | Traditional Pitfall | New Guideline Solution |
|---|---|---|
| Sinus Bradycardia | Misclassified as pathological | Recognize as physiological adaptation |
| ST Segment Elevation | False suspicion of myocarditis | Consider ethnicity and training level |
| T-Wave Inversion | Overdiagnosis of cardiomyopathy | Use supplementary imaging before diagnosis |
Expert Recommendations for Training and Implementation
To effectively enhance the accuracy of ECG interpretation in athletes, experts emphasize the importance of rigorous, standardized training protocols. Medical professionals should engage in specialized workshops that focus on the physiological adaptations unique to athletes’ hearts, differentiating normal variants from pathological findings. Key skills include:
- Recognizing training-related ECG patterns such as sinus bradycardia and early repolarization
- Identifying red flags that warrant further cardiac evaluation
- Applying athlete-specific interpretation criteria consistently
Implementation of these guidelines requires collaborative strategies within sports medicine teams. Integrating ECG review protocols into routine pre-participation screenings can significantly reduce false-positive rates while improving sensitivity. Institutions are encouraged to utilize multidisciplinary case discussions, involving cardiologists, sports physicians, and electrophysiologists, to refine diagnostic confidence. The following table summarizes the essential training components and practical steps for implementation:
| Training Aspect | Implementation Strategy |
|---|---|
| Athlete-Specific ECG Patterns | Mandatory educational modules during certification |
| Risk Stratification Skills | Routine multidisciplinary case reviews |
| Use of Updated Interpretation Criteria | Integration into electronic health record prompts |
Balancing Performance Assessment with Athlete Safety Concerns
Striking the right balance between thorough performance assessment and prioritizing athlete safety remains a critical challenge within sports cardiology. Advances in ECG interpretation now allow for more precise differentiation between physiological adaptations and potential pathological findings in athletes. This progress minimizes unnecessary restrictions or stress that overcautious evaluations might impose, while ensuring that those at genuine risk receive timely and appropriate intervention. Emphasizing a tailored, evidence-based approach enables clinicians to uphold the integrity of athletic performance assessments without compromising the well-being of the athlete.
To navigate this complex landscape, multidisciplinary collaboration and standardized protocols are essential. The new guidelines advocate for clinicians to consider athlete-specific factors such as age, ethnicity, sport type, and training intensity. Additionally, they recommend increased use of second-line diagnostic tools only when ECG findings are ambiguous. The following table highlights key changes in the revised ECG interpretation framework:
| Aspect | Previous Approach | New Guideline |
|---|---|---|
| Threshold for abnormal findings | Conservative, high false-positive rate | Refined criteria reducing false positives by 30% |
| Use of ethnicity-specific norms | Limited consideration | Mandatory for Black, Afro-Caribbean athletes |
| Follow-up testing | Broad application | Targeted, based on risk stratification |
- Improved specificity reduces athlete anxiety and unnecessary diagnostic burden.
- Enhanced safety from prompt identification of at-risk individuals.
- Streamlined processes aligned with contemporary athletic populations.
Insights and Conclusions
As the landscape of sports medicine continues to evolve, these new guidelines mark a significant step forward in refining ECG interpretation for athletes. By enhancing accuracy and reducing false positives, they promise to improve both athlete safety and performance monitoring. Dr. Babette Pluim’s insights underscore the critical role of updated protocols in bridging the gap between clinical expertise and athletic health. For clinicians and sports professionals alike, staying abreast of these developments will be essential in delivering informed, effective care.